◾Scientists say the vaccine is
getting close to human trials after being safely tested in three mammals.
https://www.utsouthwestern.edu/newsroom/articles/year-2018/dna-vaccine-alzheimers.html Monday, November 26, 2018
Positive Research on Alzheimer’s Disease
◾A DNA vaccine reduces both
harmful proteins associated with Alzheimer’s disease, without the brain
swelling caused by earlier antibody treatments.
Thursday, November 15, 2018
Over Medication in Nursing Homes
Study finds Link between Higher Registered Nurse Hours and
Lower Antipsychotic Drug Use
The federal Nursing Home Reform Law requires every nursing
facility to have a registered nurse on duty eight hours a day, seven days a
week. Despite the existence of this minimal floor for registered nurse hours,
some nursing homes still fail to meet this requirement. Data from the newly
implemented payroll-based journal (PBJ) system shows that, for at least one day
in the last quarter of 2017, 25 percent of facilities “reported no registered
nurses at work.” As many reports have indicated, quality of care and quality of
life among nursing home residents suffer when inadequate staffing exists. A
recently published report in the Journal of Psychiatric and Mental Health
Nursing (JPMHN) now lends further evidence that registered nurse hours and
antipsychotic drug use are linked.
According to “An observational study of antipsychotic
medication use among long-stay nursing home residents without qualifying
diagnoses,” increasing registered nurse hours could reduce antipsychotic drug
use among residents. The study found that just “[o]ne additional registered
nurse hour per resident day could reduce the odds of antipsychotic use by 52%
and 56% for residents with and without a dementia diagnosis respectively.”
Looking at nursing homes in the state of Missouri, the study found that meeting
the national average in registered nurse hours (.8) would reduce the odds of
inappropriate antipsychotic drug use among residents with and without dementia
by 22 percent and 25 percent, respectively.
The authors of the study concluded by stating that nursing
homes “must work to reduce APM [antipsychotic medication] use, primarily for
residents’ health, but also for certification and survey outcomes.” The authors
also encourage the use of evidence-based nonpharmacological interventions to
reduce the use of antipsychotic drugs and comply with federal regulations.
•For more information about the registered nurse hours of
any given nursing home, please see LTCCC’s nursing home staffing data for the
first quarter of 2018, available at https://nursinghome411.org/nursing-home-staffing-2018-q1/.
•To learn about resident rights in relation to
antipsychotics, please see LTCCC’s Issue Alert on antipsychotic drugs,
available at https://nursinghome411.org/issue-alert-antipsychotic-drugs/.
•To learn about the federal nursing home staffing
requirements, please see LTCCC’s Issue Alert on staffing, available at https://nursinghome411.org/ltccc-issue-alert-nursing-home-staffing-requirements/.
Thursday, November 8, 2018
Nursing Homes - Drugging of Residents; Particularly Dementia Residents
Despite Promised Crackdown, Citations for Inappropriate Drugging Remain Rare
Are States Ignoring The Impact On Vulnerable Residents? 98% of All Drugging Citations & 99.5% of Psychotropic Drugging Citations Fail to I.D. ANY Resident Harm.
New York, NY, November 8, 2018— The inappropriate antipsychotic drugging of nursing home residents, particularly those with dementia, is a widespread, national problem. These and other psychotropic drugs are too often used as a form of chemical restraint, sedating residents so that not only their behaviors but also the underlying causes for those behaviors do not have to be addressed by staff. In addition to destroying social and emotional well-being, these drugs greatly increase risks of stroke, heart attack, diabetes, Parkinsonism, and falls.
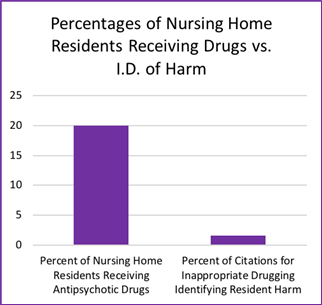
Last week, LTCCC published the Latest Drugging Rates For Every US Nursing Home. These data indicate that approximately 20% of residents - over 250,000 vulnerable individuals - are being administered powerful antipsychotic drugs in our nursing homes. Only 2% of the population will ever have a diagnosis for a condition which the government uses when it risk-adjusts for potentially appropriate use.
Today, we are announcing the release of the Latest National Data On Drugging Citations. States are required to issue a citation when a nursing home fails to meet minimum care standards. However, federal data for the last three years indicate that citation rates are very low, with significant antipsychotic drugging of residents who have dementia occurring with impunity in nursing homes across the country.
In November 2017, CMS introduced a separate citation category specifically focused on inappropriate psychotropic drugging. In addition, CMS issued new Guidance for surveyors and new survey protocols to better identify and address dangerous and inappropriate drugging. Unfortunately, continued under-enforcement means these changes have not resulted in more accountability. As the following figure shows, to date, 99.56% of all psychotropic drugging citations identify no resident harm whatsoever.

“It is very alarming that antipsychotic drugging is going up while, at the same time, states are retreating in their duty to protect both residents and taxpayer funds,” said Richard Mollot, LTCCC’s executive director. “Even in rare occasions when inappropriate drugging is identified by the state, the failure to recognize resident harm in over 98% of those cases sends a message to the nursing home industry that inappropriate drugging is okay.” Identification of harm is critical to nursing home quality assurance because, in the absence of a finding of harm or immediate jeopardy, facilities rarely face any penalty whatsoever.
In the United States, there were a total of 9,893 inappropriate drugging citations over the last three years. Only 165 of these citations identified resident harm. That is an abysmal rate of 1.56%. Meanwhile, 20% of residents receive antipsychotics, despite the nursing home industry’s six-year old campaign to improve dementia care and reduce antipsychotic drugging, and its claims that nursing homes “are getting dramatically better.”

To view drugging citations for the last three years, visit https://nursinghome411.org/us-
To view antipsychotic drugging rates for all U.S. facilities, visit https://nursinghome411.org/us-
For more information on quality of care standards, including our Dementia Care Advocacy Toolkit and fact sheets on residents’ rights, visit the Learning Center on our website at https://nursinghome411.org/
Long Term Care Community Coalition
www.nursinghome411.org
One Penn Plaza, Suite 6252
New York, NY 10119
United States
www.nursinghome411.org
One Penn Plaza, Suite 6252
New York, NY 10119
United States
Tuesday, November 6, 2018
Drugs and Healthcare
 |
When Do Drug and Healthcare Ads Push Ethical Boundaries?
You’d be right if you suspect that drug makers are spending A LOT more on TV advertising. Pharmaceutical companies have more than doubled ad spending in just the past four years, making it the second-fastest growing ad category in the nation. Other healthcare providers – from local hospitals to nationally-known cancer treatment centers – are also upping the advertising ante. But when do healthcare promotions cross ethical boundaries and the ancient pledge to all patients of “do no harm?” You should know!
| POSITIVE BUT PAINFUL ADSSome patients say healthcare ads that feature happy, healed people and miraculous recoveries spread false hope. http://letamericaknow.com/view_newsletter_ysk.php?memberid=28&orderid=39&issueid=1811 | ||||||
Friday, November 2, 2018
Drugging of Nursing Home Residents
Media Advisory: Latest Federal Data Reveal Widespread Antipsychotic Drugging of Vulnerable Nursing Home Residents
Despite Industry’s Claims of “Success” in Reducing Drugging, Rates Have Gone Up; Approx. 20% of Residents STILL Receiving Powerful, Potentially Lethal Meds
New York, NY, November 1, 2018— The inappropriate antipsychotic drugging of nursing home residents, particularly those with dementia, is a widespread, national problem. Despite the Food and Drug Administration’s ‘black box’ warnings against using antipsychotics on elderly patients, they are frequently used to treat the so-called behavioral and psychological symptoms of dementia.
These and other psychotropic drugs are too often used as a form of chemical restraint, sedating residents so that not only their behaviors but also the underlying causes for those behaviors do not have to be addressed by staff. In addition to destroying social and emotional well-being, these drugs greatly increase risks of stroke, heart attack, diabetes, Parkinsonism, and falls. They are not clinically indicated for dementia-related psychosis. They are associated with a significant increase in death when given to elderly people with dementia.
Today, we are announcing the release of the Latest Drugging Rates for Every US Nursing Home. These data indicate that approximately 20% of residents - over 250,000 vulnerable residents - are being administered powerful antipsychotic drugs in our nursing homes today. Only 2% of the population will ever have a diagnosis for a condition which the government uses when it risk-adjusts for potentially appropriate use. “Too many residents and families are not even made aware of the dangerous potential side-effects of these drugs, or the fact that they are not clinically indicated for so-called dementia “behaviors,” said Richard Mollot, LTCCC’s executive director.
In addition to data on nursing home drugging rates, LTCCC’s website, www.nursinghome411.org, has a range of information and resources for consumers and the public, including:
Issue Alert on Antipsychotic Drugs: This alert explains how and why this is a significant issue for so many nursing home residents. It includes a case study of a citation for inappropriate antipsychotic drugging.
Dementia Care Advocacy Toolkit: Free resources to help families, and those who work with them, know their rights and advocate for less drugging and better care for their residents with dementia.
Monthly Webinars: On the 3rd Thursday of every month we hold a free “lunch-and-learn” program open to all stakeholders on residents’ rights and quality of care issues.
LTCCC is a nonprofit organization dedicated to protecting the rights and welfare of long term care consumers in all settings, including nursing homes, assisted living facilities and in their communities, by strengthening regulation, surveillance and enforcement.
For more information on this and other long term care issues, visit www.nursinghome411.org.
Long Term Care Community Coalition
www.nursinghome411.org
One Penn Plaza, Suite 6252
New York, NY 10119
United States
www.nursinghome411.org
One Penn Plaza, Suite 6252
New York, NY 10119
United States
Subscribe to:
Posts (Atom)
